In an eggshell...
- An ovarian stimulation protocol is a medication or treatment regimen that ‘stimulates’ the ovaries
- There’s no ‘one size fits all’ protocol
- Your stimulation protocol will depend on your medical history, response, and hormonal levels
If you’re starting an egg freezing cycle, you’ll probably start hearing these terms:
Stimulation. Protocol. Gonadotropins. FSH. LH. Dominant follicle.
Now, before you start fumbling around for a glossary of these terms, we’ve got you.
This is the DIY part of the cycle, essentially- where you get the medication, start your cycle, the ultrasound appointments- the nitty gritty of it all.
And more than anything, knowing what you’re facing, be it the protocol, the type of medication you’re taking or even your hormonal fluctuations throughout the cycle really help.
We sat with our in-house medical team, to really understand how protocols are personalised, the common ones and how medications work during the cycle to maximise the number of eggs you retrieve.
So, grab that mug of coffee and settle in!
What is an Ovarian Stimulation Protocol?
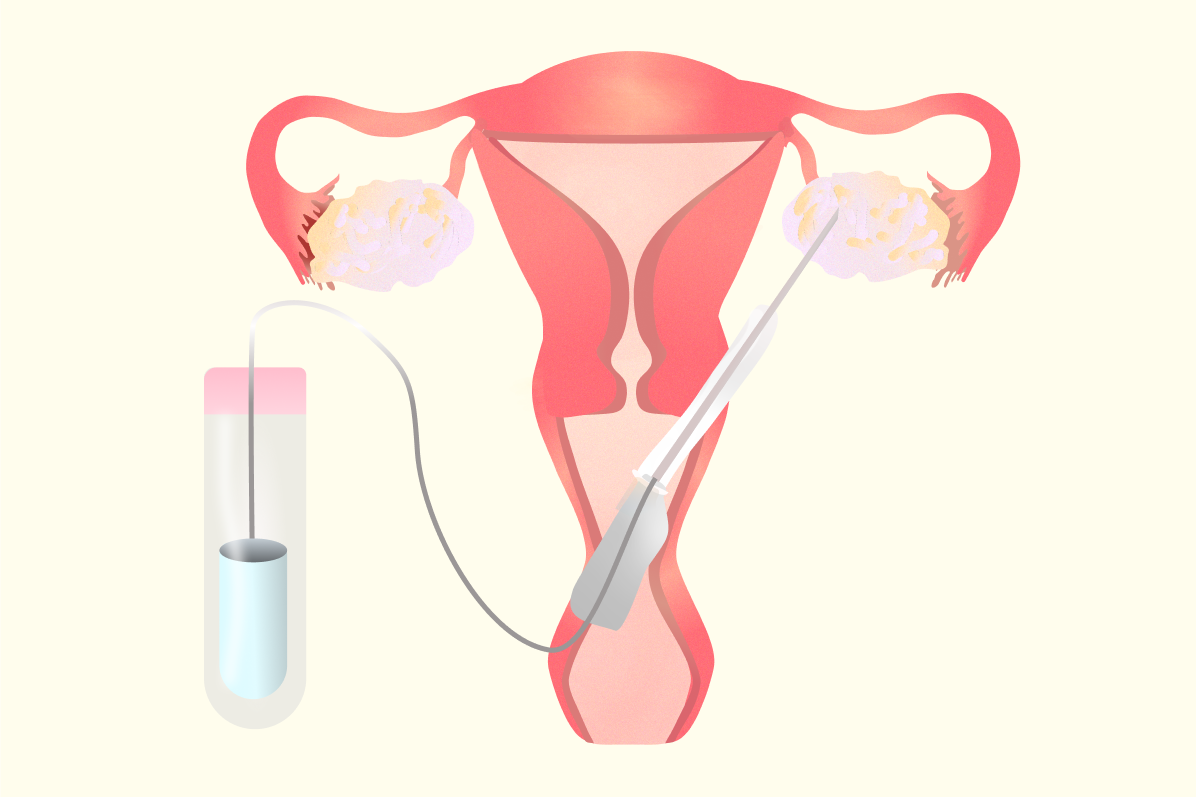
An ovarian stimulation protocol is a medication or treatment regimen that ‘stimulates’ the ovaries to recruit more follicles to grow during a particular cycle.
This is done with the aim to retrieve mature eggs from these follicles during the egg freezing cycle.
Every ovarian stimulation protocol essentially ends with the trigger injection, which helps mature the eggs. The egg collection surgery happens 34-36 hours later, to collect the mature eggs, which are then frozen later on.
Will my Stimulation Protocol be the Same as Everyone else’s?
Here’s the main thing: there is no one-size-fits-all, regimen, anywhere.
Your stimulation protocol will be designed specifically for your medical history, response, hormonal levels and any other considerations if needed.
While the protocol itself might differ, most parts of it remain the same, such as:
- Monitoring throughout the protocol (blood tests and ultrasound scans)
- Doctor consultations to discuss progress and protocol modification if needed
- Trigger shot
- Egg retrieval
Types of Ovarian Stimulation Protocols
While your protocol is ultimately personalised based on your medical history, there are some common protocols that are used, and also can help you understand the fundamentals of your specific protocol as well.
So, we sat down with our medical advisor, Dr Vivienne Hall, to outline some of the most common ovarian stimulation protocols used in the UK:
1. Short Antagonist Protocol
The Short Antagonist Protocol is currently the most commonly used ovarian stimulation protocol in the UK.
It has a shorter treatment duration and uses your natural menstrual cycle to maximise egg yield while minimising risks.
How It Works
🎬 Start of Stimulation: You begin injecting stimulating hormones (FSH or follicle stimulating hormone, sometimes combined with LH or Luteinizing hormone) on day 2 of your period. Common drugs include:
- Gonal-f
- Pergoveris
- Menopur
- Bemfola
- Fostimon
⏰ Duration: The stimulation phase typically lasts 9 to 15 days, with an average of about 11 days.
➕ Adding the Antagonist: Around midway through stimulation (usually when follicles reach 12-14 mm), a second drug called a GnRH antagonist (common ones include Cetrotide and Fyrenedel) is introduced.
This medication blocks the receptors that cause an LH surge, preventing premature ovulation before egg retrieval.
💉 The Trigger Injection
When the follicles have matured (usually around 18-20 mm), a trigger injection is given to initiate the final maturation of eggs and prepare them for collection.
This injection is given once, typically 36 hours before egg retrieval.
Some examples of trigger drugs:
- Gonasi (HCG)
- Zivafert
- Ovitrelle
- Buserelin
Sometimes, two triggers are given together (e.g., two doses of Zivafert or Ovitrelle), or a combination like Buserelin plus Zivafert. Occasionally, triggers are given a few hours apart in a staggered trigger approach. This is followed by egg retrieval and freezing.
2. Long Suppression Protocol
The Long Suppression Protocol is a controlled ovarian stimulation protocol to prevent premature ovulation and allow precise control over the timing of egg retrieval.
“This protocol means you have more injections for a longer time, but it is useful for programming cycles in advance and is often used with the contraceptive pill to give complete control and advanced planning” says Dr Vivienne. “However, it is not recommended in patients with polycystic ovaries”
This is mostly due to the fact that PCOS patients are at higher risk of ovarian hyperstimulation syndrome (OHSS) and may not respond well to prolonged suppression. Instead, alternative protocols like the antagonist protocol are preferred for better safety and flexibility in PCOS.
How It Works
🎬 Starting the Agonist (GnRH Agonist) Injection
- You begin injecting a GnRH agonist (examples: buserelin, Synarel) on day 21 of your menstrual cycle, which is typically about a week before your period starts.
- This early start is designed to "downregulate" your pituitary gland.
🧠 Pituitary Down Regulation
- The GnRH agonist initially causes a brief surge in luteinizing hormone (LH) and follicle-stimulating hormone (FSH), but continued use suppresses the pituitary gland.
- This suppression prevents your body from releasing its own LH and FSH, effectively stopping natural ovulation.
- Because your pituitary is "turned off," there is no risk of premature egg release during the stimulation phase.
🎬 Starting Ovarian Stimulation
- After confirming pituitary suppression (usually after 10-14 days), you start ovarian stimulation with injectable FSH or hMG to promote follicle growth.
- Since the pituitary is suppressed, the follicles develop only in response to the medications you administer, giving your doctor full control.
The cycle then ends with the trigger injection and egg retrieval as planned.
Also read: I have PCOS, can I freeze my eggs?
3. Flare Protocol
The Flare Protocol is designed for patients with a low ovarian reserve or those who have had a poor response to previous IVF or egg freezing cycles.
It uses the initial stimulating effect of a GnRH agonist to “flare” or recruit more follicles.
How It Works
🎬 Start of Treatment: You start injecting a GnRH agonist (e.g., Buserelin or Synarel) on day 1 or 2 of your period, along with stimulation drugs such as Gonal-f.
- The GnRH agonist initially causes a flare-up of natural LH and FSH release from the pituitary, which helps recruit more follicles early on in the cycle.
- This protocol aims to maximise the number of follicles recruited, potentially increasing the number of eggs collected.
However, this protocol may have a higher risk of premature LH surge compared to antagonist protocols, so timing and monitoring are critical. The stimulation phase is then followed by trigger and egg retrieval.
4. Natural Modified Protocol
The Natural Modified Protocol is a highly specialised approach used for women with a critically low ovarian reserve.
It relies on the body’s natural selection of a dominant follicle and supports it with minimal stimulation.
How It Works
- The protocol monitors your natural menstrual cycle to identify the dominant follicle.
- A very low dose of stimulation drugs is given to support the growth and maturation of this single follicle.
- Typically, only one egg is collected per cycle.
- This approach helps reduce medication exposure and focuses resources on the best-quality egg available naturally.
While this protocol is suitable for women with very low egg reserve or advanced maternal age, it does require precise timing and close monitoring as there is less medications, thus less control over the cycle.
It also has fewer side effects compared to full stimulation protocols.
Also read: Can I improve egg quality before egg freezing?
Factors that Influence Your Ovarian Stimulation Protocol
The primary goal of any stimulation is the same: to safely stimulate the ovaries to produce multiple mature eggs for retrieval and freezing.
But, to do that, there are some factors that doctors consider. Here’s a breakdown of the main ones:
🧓 Age
This is one of the most important factors that affect how your stimulation protocol is designed. The main cause behind this is that as a woman ages, her ovarian reserve (the number and quality of remaining eggs) declines.
Essentially, the ovarian reserve of a 25-year-old looks very different from that of a 40-year-old. Older women (typically late 30s and older) often require higher doses of stimulation medications (gonadotropins). But the same, if given to younger women may cause a hyper response.
This is why age factors in majorly while designing your stimulation protocol.
📈 Ovarian reserve markers
Ovarian reserve markers such as AMH (Anti-Mullerian Hormone) and AFC (Antral follicle count) give us an idea of the potential egg supply.
A high or low ovarian reserve can also factor in while deciding your protocol. Here’s why:
- High Ovarian Reserve: Women with conditions like polycystic ovary syndrome (PCOS) often show elevated AMH levels and high AFC, which puts them at a risk of hyper response and increased risk of OHSS.
In these cases, protocols typically start with lower doses of gonadotropins and may use alternative triggers to reduce OHSS risk.
- Low Ovarian Reserve: Women with low AMH and AFC often show poor ovarian response. For these patients, higher doses of gonadotropins may be necessary, and sometimes, adjunctive medications like growth hormone are considered to improve outcomes
💉 Previous Response to Ovarian Stimulation
If you’ve undergone an egg freezing cycle in the past, or are on your second or third round, your response in your previous cycles is, in a way, a guide for your doctor.
Here’s how:
- Poor Response: If your previous cycle yielded fewer eggs than expected, your doctor may increase gonadotropin doses or adjust the medication type to improve response in subsequent cycles.
- Over Response: If you had an excessive response previously, the protocol may be modified to use lower doses or different medications to reduce the risk of OHSS and other complications.
💊 Underlying Medical Conditions
Several underlying medical conditions can influence your stimulation protocol and might require personalisation:
Polycystic Ovary Syndrome (PCOS)
Women with PCOS have high antral follicle counts and elevated AMH levels, and are at a risk of ovarian hyperstimulation syndrome (OHSS).
For PCOS patients, protocols typically favour GnRH antagonist regimens with lower gonadotropin doses and agonist triggers. Adjunct treatments like metformin may also be recommended to improve insulin resistance and reduce OHSS risk.
Endometriosis
This condition can sometimes impact ovarian reserve or ovarian responsiveness, potentially due to inflammation, endometriomas (cysts on the ovaries), or previous surgeries.
Depending on the severity and location, it might influence egg quality or the number retrieved. For endometriosis, the protocols may involve changes in the dosage based on response, or pre-treatment with medication to subside the side effects and maximise results.
Thyroid Disorders
Conditions like Hashimoto's thyroiditis (where your immune cells attack the cells of your thyroid gland) can be complicated during ovarian stimulation.
The stimulation medication can increase estrogen levels, which then increases the production of TBG, a protein that binds to thyroid hormones in the blood. Due to this, the amount of "free" (active) thyroid hormone available to the body decreases, leading to complications such as subclinical hypothyroidism.
In such cases, the protocol is modified along with an adjustment in thyroid medication before and during stimulation to reduce risk.
Genetic Factors such as FSHR Polymorphism
Your genetic makeup can affect how your ovaries respond to FSH hormones.
For instance, FSHR polymorphism is one such genetic variation which makes women’s ovaries less responsive, requiring higher medication doses. Interestingly, treatments like growth hormone have been found to work well in patients with genetic variants such as FSH polymorphisms. Ultimately, conditions like these could lead to modifications in your specific protocol.
How Amilis Can Help You on Your Fertility Journey
Knowing you’re in the right hands, or having the right support, matters at every stage of your fertility journey.
Be it during your scans, fertility testing, or up until egg retrieval, every step matters. The clinic you visit, the support you have and the doctors you trust during your cycle.
That’s why at Amilis, we’ve made it our priority to provide the best care at every stage of your cycle.
Here’s how we do it:
- Zero waiting times to test your fertility. Book a fertility test anytime, at your convenience.
- A full hormone panel at just £130 and an AMH test for just £80 (50% cheaper than fertility clinics)
- A personalised report on your hormone levels and what they could mean for your fertility
- Book free consultations with expert doctors to discuss results and next steps
- Book free consultations with the best fertility clinics across the UK
When you opt to start your fertility journey via Amilis, you also get a stellar support team (that’s us 👋) guiding you along at every step!
Figuring out where to get started? Book a doctor consultation or take our personalised fertility quiz to know more!






.png)

