Contents
- What is OHSS?
- What causes OHSS?
- When does OHSS start after egg retrieval?
- How long does OHSS last?
- Does OHSS affect egg quality?
- Symptoms of OHSS after egg retrieval
- How do I know if I’m at risk of OHSS?
- How to Prevent OHSS in Egg Freezing Cycles
- How is OHSS treated?
- Get Expert Fertility Care in the UK, via Amilis
- Frequently asked questions
In an eggshell...
- OHSS is a risk associated with egg freezing, where the ovaries overproduce eggs and swell up
- There’s no exact reason behind it, but doctors monitor symptoms and vitals to check for any warning signs
- Your medical history and genetics can play a part in whether you are at risk of OHSS
- OHSS is preventable- and treatable.
Egg freezing, like every other procedure, comes with a fair share of minor risks.
So your brain gets working to direct the ovaries to produce more eggs than usual.
But sometimes, the ovary can hyper-respond. It gets into egg-producing mode, to the point where it gets a little risky for the body.
That's OHSS or Ovarian Hyperstimulation Syndrome.
We get it, as someone who’s thinking of an egg-freezing cycle, you may be confused if you’ve come across this term. But we’re here to give you all the insider information on what it is, and how it's preventable.
Read on!
What is OHSS?
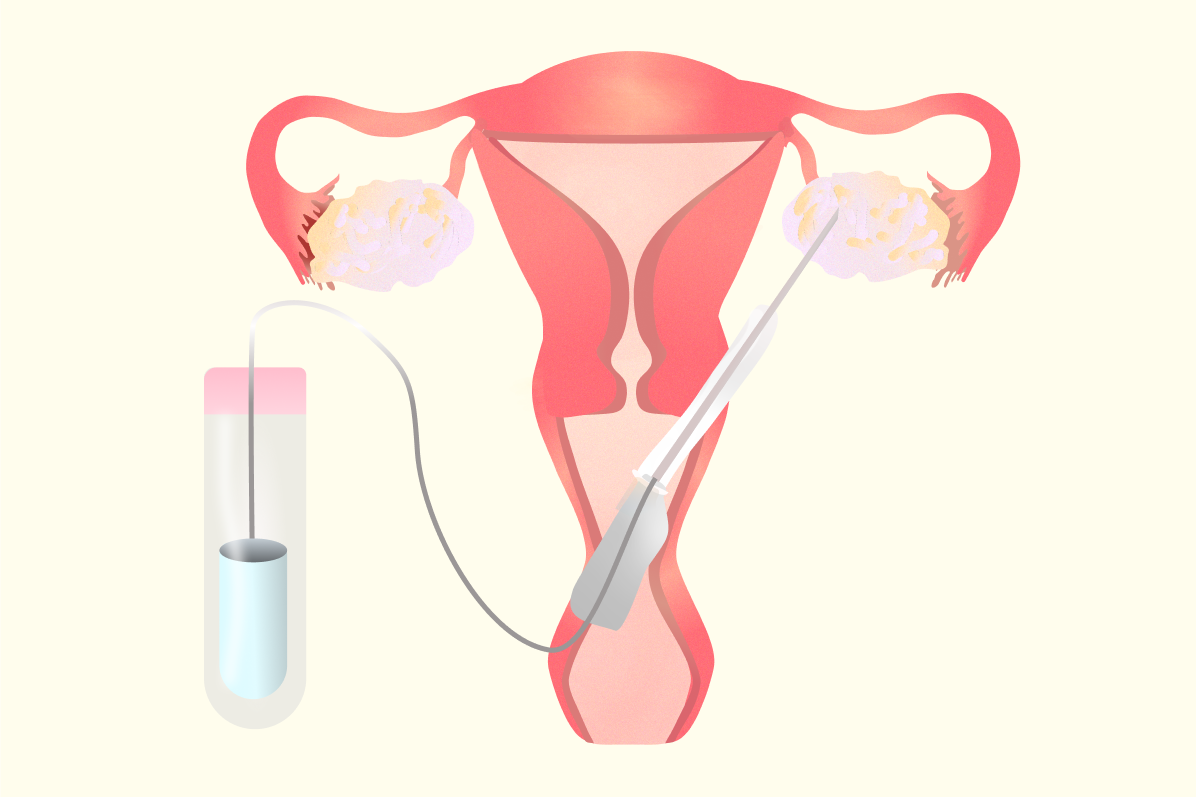
OHSS is one such risk associated with egg freezing, where the ovaries tend to swell up due to overproduction of eggs, along with pain and fluid retention in the abdomen.
It happens when the ovaries produce high levels of a protein called VEGF after being stimulated by fertility medication. VEGF increases the permeability of tiny blood vessels, causing fluid to leak from blood vessels and into places like the abdomen or chest.
This fluid build-up can cause bloating, discomfort, and sometimes pain. The more the vessels leak, the more severe the symptoms can be.
Are there types of OHSS?
There are three types- mild, moderate, and the least common one, severe.
Mild to moderate cases have lesser symptoms and are often managed with outpatient treatment. This could mean repeated visits to the doctor after your egg retrieval, to check on your vitals, and intake medication until your period comes in.
But in severe cases, you may be redirected to a doctor specialised in managing severe OHSS.
You start the cycle with medication that tells your ovaries “hey we need to grow more eggs this time, and we need to catch ‘em all” 👮
Let's take a realistic view of it. As per studies, the incidence of OHSS is anywhere between 3.1 and 8%, but can be up to 20% in high-risk women (that is, women who have pre-existing conditions that put them at risk or have a previous history of OHSS)
What causes OHSS?
Well, this is a puzzle for scientists too🧩
There’s no single cause behind OHSS. For instance, the egg freezing trigger shot given to mature the eggs before egg retrieval is known to be a cause.
On the other hand, it can also happen with the usage of gonadotropins, which is usually given during the stimulation phase of your egg-freezing cycle.
So the cause of OHSS may be different, depending on the case. But it’s almost always detectable.
When does OHSS start after Egg Retrieval?
OHSS typically peaks around 5-10 days after an egg retrieval.
This is because your egg-freezing cycle involves “stimulating” the ovaries to produce more eggs. Stimulation involves medications and hormonal triggers.
These medications and triggers are known to be a major cause of OHSS. And since they hang around in your system for quite a while, even after the egg retrieval, they can put you at risk for OHSS.
How long does OHSS last?
In mild to moderate cases, OHSS usually lasts about 7 to 10 days, and symptoms often clear up within this time if you are not pregnant.
If pregnancy occurs, especially if you’ve had a fresh embryo transfer (aka an embryo transfer 2-5 days after egg retrieval), or if it’s a late-onset OHSS, symptoms can last longer. It may also get triggered by the rising hCG released by the placenta.
Recovery time also depends on how severe your OHSS is and factors like having polycystic ovary syndrome (PCOS).
In hospital-treated cases or severe OHSS, most people recover in about 11 days, but it can take longer for some. OHSS generally goes away on its own, with treatment aimed at easing symptoms and preventing complications until your body recovers.
Does OHSS affect egg quality?
No, in most cases, OHSS does not affect egg quality.
But what it could affect is the quantity. OHSS could lead to more number of eggs being retrieved than usual.
But there’s a catch. A smaller proportion of them may be high quality. Fertilisation rates can also be a bit lower compared to people who don’t develop OHSS.
But the good news is that embryo quality, implantation rates, and pregnancy rates are usually not affected much. So even if some eggs aren’t perfect, your chances of success can still be very similar.
Symptoms of OHSS after Egg Retrieval

So, how exactly do you know if you have OHSS?
Given that there are hormonal tests done right before your egg retrieval, there are some telltale signs of OHSS that healthcare providers can look out for (more on that below).
However, the symptoms of OHSS depend on the severity of the condition. Here are some symptoms to look out for:
Mild OHSS Symptoms
- Mild abdominal swelling and discomfort
- Nausea and occasional vomiting
- Enlarged ovaries (5 to 8 cm) without significant fluid accumulation
Moderate OHSS Symptoms
- Symptoms of mild OHSS plus abdominal bloating from fluid buildup (ascites), which is detectable on ultrasound
- Nausea, vomiting, diarrhoea, and mild to moderate abdominal pain
- Ovarian enlargement up to 12 cm
- Rapid weight gain (>3 kg) may occur
Severe OHSS Symptoms
- A large build-up of fluid in the tummy or chest, which can cause swelling, bloating, and trouble breathing
- Very little or no urine output (less than about a cup in a whole day)
- Feeling dehydrated, dizzy, or weak
- Blood becomes thicker than normal, which can raise the risk of blood clots
- Very large ovarian cysts (over 12 cm) that may cause pain
- In some cases, the kidneys or liver may not work properly
But here’s the thing: Severe OHSS is as rare as it comes. Only about 1 in 100 women may develop moderate or severe OHSS.
When should I Seek Medical Attention with OHSS?
Ideally, it's best to reach out to your healthcare provider if you feel that your OHSS symptoms aren’t receding. If you feel dehydrated, vomiting, have discomfort or are having difficulty passing urine, it’s better to get some additional care at the hospital.
This can ensure that your symptoms subside faster, and you’re back on the road to recovery.
How do I know if I'm at risk of OHSS?
Certain factors can make OHSS more likely, and healthcare providers often check for these before starting treatment. This way, the stimulation protocol can be adjusted to minimise risk.
Some risk factors include:
- Younger age – particularly under 30–35 years, as the ovaries often respond more strongly to stimulation
- Lower body mass index (BMI) – research shows an inverse relationship between BMI and OHSS risk
- Polycystic ovary syndrome (PCOS) – linked to higher AFC (Antral Follicle Count) and AMH (Anti-Mullerian Hormone) levels, which increase ovarian sensitivity
- High baseline antral follicle count – typically more than 17 or 24 follicles, depending on the study
- Elevated AMH levels – often above 3.5 ng/mL, with some studies using higher cut-offs
- Rapidly rising or high estradiol (E2) levels – above around 3,500–5,000 pg/mL during stimulation
- Large number of follicles at trigger – usually more than 15–18 follicles on the day ovulation is triggered
- Use of hCG for triggering ovulation – carries a higher OHSS risk compared to GnRH agonists
- High doses of gonadotropins – stronger ovarian stimulation can raise risk
- History of OHSS – previous episodes increase the likelihood of recurrence
- Possible genetic predisposition – Studies are investigating certain FSH receptor or FLT4 gene variants as a possible cause of OHSS
- Allergies or hypersensitivity – These are also some potential contributors which are still being researched
How to Prevent OHSS in Egg-Freezing Cycles?
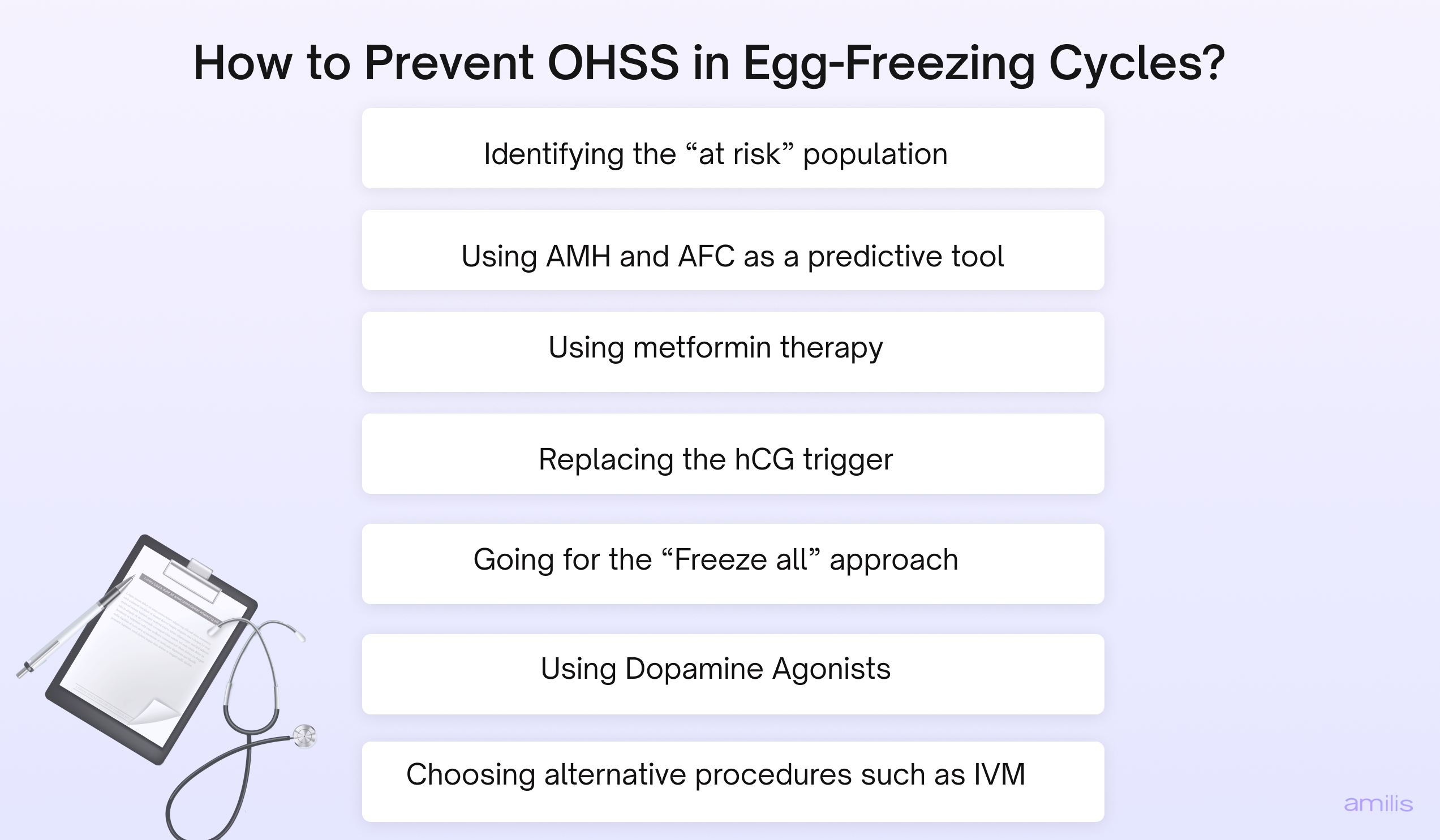
While there’s no single signal that can predict OHSS, almost all prevention strategies involve attentive, personalised care and adjusting the dosage of medications accordingly.
OHSS can be prevented in egg-freezing cycles by following a mix of monitoring and strategies, such as:
Identifying the “at-risk” population
Being aware of the patients at risk can help clinicians modify protocols, such as reducing the dosage of gonadotropins, from the start, and avoid the occurrence of OHSS
Using AMH and AFC as a predictive tool
Studies mention that AMH levels >3.36ng/mL before an egg freezing cycle could indicate a risk of OHSS. For reference, AMH levels of 1-3 are considered normal and not at risk.
Similar to AMH, an AFC level of >24 can be a predictor of moderate to severe OHSS. This way, healthcare providers can be more vigilant of your response in the egg-freezing cycle.
Using metformin therapy
Metformin therapy, especially in women with PCOS, may reduce OHSS risk by inhibiting the secretion of VEGF, lowering vascular permeability and hormone levels like progesterone and estradiol during stimulation.
Replacing the hCG trigger
In egg freezing cycles, 36 hours before your egg retrieval, a hCG trigger is given to mature the eggs.
But the effects of hCG stay in the body for longer, increasing the risk of OHSS. Instead, replacing the egg freezing trigger with an alternative such as GnRH agonist or recombinant LH can reduce the risk of OHSS by shortening the LH surge or inhibiting the secretion of VEGF.
Going for the “Freeze all” approach
A “freeze-all” approach means freezing all eggs or embryos after retrieval and waiting to do the embryo transfer in a later, natural cycle.
This helps avoid the hormone changes in early pregnancy that can trigger late-onset OHSS. By removing that pregnancy-related hCG surge, the risk of late OHSS is almost completely eliminated.
Using Dopamine Agonists
Dopamine agonists such as cabergoline used around the trigger time or from the day of trigger have also shown efficacy in reducing the severity of OHSS by blocking VEGF receptors.
Choosing alternative procedures such as IVM
IVM or In vitro maturation is a method where immature eggs are retrieved from your ovaries and matured in the laboratory, before freezing. This requires little to no stimulation medication, thus reducing the risk of OHSS.
So with all this in mind, clinics work on providing personalised protocols. If they detect any of these factors during the monitoring and treatment stage, your protocol may be tailored further to help stimulate your eggs, but largely minimise the risk of OHSS.
How is OHSS treated?
Mild to moderate OHSS symptoms usually resolve with medication, treatment, and lots of rest. You may have regular consultations, an ultrasound, and blood tests to ensure that your symptoms don't worsen. Some of the treatments include:
Drinking plenty of fluids
As OHSS causes dehydration and a decrease in urine output, electrolyte-supplemented drinks, and water are recommended such that your urine becomes pale yellow. Refrain from sodas or any other caffeinated drinks while you recover.
Say no to strenuous activity
It’s best to rest and recover after an egg-freezing cycle. You will usually be recommended to not engage in heavy exercise or lift weights for about 48 hours until a week for good measure.
Eat nutritionally healthy food
It's advised to avoid oily, junk food and switch to leafy greens and a protein-rich diet, as recommended by your healthcare provider.
Take prescribed medications
You may be prescribed pain relievers, anti-nausea medications, and diuretics to drain excess fluid from the abdominal region.
If you do happen to develop severe OHSS, you may require hospitalisation and treatment. This involves:
- A thorough investigation, such as CBC, liver function test, serum oestrogen levels, etc
- Heart rate and blood pressure checkups
- Daily assessment of BMI
- Intravenous fluids
- Electrolyte replacement
This can help prevent complications such as dehydration and blood clots. And even at this stage, bed rest and good fluid intake are at the top of the priority list!
Get Expert Fertility Care in the UK, via Amilis
When you choose the right specialist, clinic, and the white resources, your fertility journey becomes a tad bit easier.
Especially when you’re starting out, it can look like a maze. Having the right resources at this stage can improve your entire egg freezing experience.
That’s why, at Amilis, we believe in providing the best care, from the very first step. Here’s how:
- Book an AMH test for just £80 and a full hormone panel for £130 (50% cheaper than fertility clinics)
- Get free consultations with expert doctors across the UK
- Free consultations with vetted egg freezing clinics near you
- Free 1-1 calls with Amilis experts throughout your journey
It’s about time we make fertility care accessible, not a luxury.
And we’re paving the way for it, one day at a time 🙌🏼
Frequently asked questions
How soon after egg retrieval does OHSS occur?
OHSS can appear quite soon after egg retrieval. Early-onset OHSS usually shows up within 3 to 7 days, triggered by the hCG injection used to mature the eggs. Late-onset OHSS tends to happen around 10 days after retrieval and is often linked to pregnancy hormones.
Can you still have an embryo transfer with mild OHSS?
Mild OHSS usually doesn’t stop an embryo transfer from going ahead, and many clinics will proceed with careful monitoring. If symptoms are moderate or severe, the safer option is to freeze the embryos and delay transfer until a later cycle. This helps prevent symptoms from getting worse.
How long does it take for OHSS to resolve?
In most cases without pregnancy, OHSS improves within 7 to 10 days. If pregnancy occurs, symptoms can last longer and may even become more intense for several weeks. Recovery time depends on the severity and how the body responds to treatment.
How to prevent OHSS after egg retrieval?
Prevention starts before OHSS develops, by tailoring the stimulation plan to reduce risk. This can include using a GnRH agonist trigger instead of hCG, monitoring hormone levels closely, and sometimes freezing all embryos to transfer later. These steps help avoid the hormone surges that make OHSS worse.
How to reduce OHSS bloating?
Mild bloating can often be eased by staying well-hydrated, resting, and avoiding heavy exercise. Wearing loose clothing and eating smaller meals may also help with comfort. In more serious cases, a doctor may drain the extra fluid from the abdomen to relieve pressure and pain.
When to go to the hospital with OHSS?
Seek urgent medical help if OHSS symptoms suddenly get worse. Warning signs include severe tummy pain, constant vomiting, passing very little urine, difficulty breathing, or swelling in the legs (which can signal a blood clot). These can be signs of severe OHSS and need prompt attention.
Can I have a successful pregnancy with OHSS?
Yes, you can have a successful pregnancy with OHSS, and many people go on to have healthy pregnancies after OHSS. Even in severe cases, with the right care and monitoring, pregnancy outcomes are usually good. The key is close follow-up to keep both parent and baby safe.






.png)

